Featured Scientist

Tsung-Tai Chen, Ph.D.
Professor
Which hospitals are better: Two hospital profiling activities, pay-for-performance (P4P) programs and quality report cards in Taiwan
Dr. Tsung-Tai Chen (陳宗泰) received a B.S. degree in Public Health, a M.S. degree in Health Policy Management, and a Ph.D. degree in Health Care Administration–all were from National Taiwan University. He is currently an Associate Professor in the Department of Public Health at Fu Jen Catholic University, Taiwan. In 2016, he went to the Melbourne School of Population and Global Health, University of Melbourne (14th on the World University Rankings 2022 by subject: clinical, preclinical & health) as a visiting scholar for 7 months. He is also currently serving as Chief Executive Officer of the Micro Program in Interdisciplinary Healthcare Service Design Thinking (輔大跨域醫療服務設計思考微學程), and Supervisor Board Member of the Taiwan College of Healthcare Executives (台灣醫務管理學會).
As a first or corresponding author, he has published several articles in well-known journals such as Value in Health, Medical Decision Making, Health Services Research (2 articles), the European Journal of Public Health, and Resuscitation.
During his research career from doctorate up to now, Dr. Chen has focused on performance measurement, especially for profiling-related research. In healthcare, well-known profiling activities include pay-for-performance (P4P), public report cards/private performance feedback. Dr. Chen’s research includes a series of goals and plans, and the article below describes his central research topics in regard to the two abovementioned profiling activities.
1 Pay-for-Performance
Dr. Chen and his advisors Prof. Kuo-Piao Chung and Prof. Mei-Shu Lai first published a detailed review article regarding P4P in 2007. This article described the design of P4P methods and made suggestions for future research, which provided a guidance in P4P policy design and ideas for Taiwanese scholars to further work on this issue.
Tsung-Tai Chen, Mei-Shu Lai, Kuo-Piao Chung*. Just another trend in healthcare? A perspective on pay for performance programs. Taiwan Journal of Public Health 2007 26(5):33-70 (TSSCI) (In Chinese).
(1) P4P design 1: Avoiding cherry picking (unintended consequences)
In 2011, Dr. Chen and Prof. Chung published an important article, which today has been cited approximately 100 times. Taiwan has instituted a P4P program for patients with diabetes that rewards physicians based in part on patient outcomes, and physicians are permitted to choose which of their patients with diabetes are included in the P4P program. In their research, Dr. Chen and Prof. Chung tested whether seriously ill patients with diabetes are disproportionately excluded from the P4P program. Based on this research, they found that patients with diabetes are disproportionately excluded from P4P programs; they point to the importance of mandated participation and risk adjustment measures in P4P programs.
Tsung-Tai Chen, Kuo-Piao Chung, I-Chin Lin, Mei-Shu Lai*. The Unintended Consequence of Diabetes Mellitus Pay-for-Performance (P4P) Program in Taiwan: Are Patients with More Comorbidities or More Severe Conditions Likely to Be Excluded from the P4P Program? Health Services Research 2011 46(1 Pt 1):47-60.
(IF=3.40; 2020 SSCI: Health Policy & Services, 16/88 [18%, Q1], The Ministry of Science and Technology [MOST] ranking in management I field: tier I)
(2) P4P design 2: Designing a composite score
While profiling hospital performance, one of the challenges is, for example, present in the care of patients with diabetes: if a hospital receives a higher grade on one outcome measure, but a lower grade on another outcome measure, a conclusion about the overall quality of this hospital cannot be made. Yet, by making a composite score based on a rigid weighting scheme, a summary of each hospital’s quality can easily be understood and tracked over time. However, the issue is that when it comes to non-latent and latent composite scores constructed using several measures for P4P, we still do not clearly understand which one are better and what their characteristics are.
In 2012, Dr. Chen and Prof. Chung published a research comparing composite scores for P4P. They found that the latent methods were superior to the non-latent methods as they were more reliable and had specific weighting themes. The correlations among the 3 latent methods were moderately high. Additionally, the use of the PRIDIT approach, which is moderately difficult compared to the item response theory–based model, is recommended if the insurer wants to balance convenience and precision.
Tsung-Tai Chen, Mei-Shu Lai, I-Chin Lin, Kuo-Piao Chung*. Exploring and Comparing the Characteristics of Nonlatent and Latent Composite Scores: Implications for Pay-for-Performance Incentive Design. Medical Decision Making 2012 32(1):132-44.
(IF=2.58; 2020 SSCI: Health Policy & Services, 42/88 [47%, Q2])
(3) P4P design 2: Designing a pay-for-performance for patient (P4P4P) program
In 2015, Dr. Chen tried to pilot evaluation regarding the possible design of a program where the incentive is to be changed and given to patients. These kinds of programs are known worldwide as pay-for-performance for patient (P4P4P) programs, but still are in its infancy in Taiwan. Dr. Chen elicited a patient's willingness to participate in a diabetes P4P4P program using a discrete choice experiment method. He found that patients with more disadvantageous characteristics (e.g., elderly, low income, greater comorbidity, and severity) would have less to gain from participating in the program and thus required a higher monetary incentive to compensate for the disutility caused by participating in the program's activities. This research demonstrates that a modest financial incentive could increase the likelihood of program participation.
Tsung-Tai Chen*, Tao-Hsin Tung, Ya-seng (Arthur) Hsueh, Ming-Han Tsai, Hsiu-Mei, Liang, Kay-Lun Li, Kuo-Piao Chung, Chao-Hsiun Tang. Measuring preferences for a diabetes Pay-for-Performance for Patient (P4P4P) program using a discrete choice experiment. Value in Health 18(2015):578-586.
(IF=5.728; 2020 SSCI: Economics, 23/376 [6%, Q1], The Ministry of Science and Technology [MOST] ranking in management I field: tier II)
(4) P4P design 3: Incentive magnitude vs. incentive form/structure
In 2015, Dr. Chen and Prof. Chung wanted to determine whether the magnitude of incentives or other design attributes should be prioritized, and aimed to find which attributes are the most important by using the discrete choice experiment method. Following this, they found that physicians may feel that good P4P designs (incentive form/structure) are more important than the magnitude of the investment by the insurer. The two most important P4P designs include providing a bonus-type incentive and using pay-for-excellence combined with pay-for-improvement.
Tsung-Tai Chen, Mei-Shu Lai, Kuo-Piao Chung*. Participating physician preferences regarding a pay-for-performance incentive design: A discrete choice experiment. International Journal for Quality in Health Care 2016 Feb 28(1):40-6.
(IF=1.829; 2020 SSCI: Health Policy & Services, 64/88, The Ministry of Science and Technology [MOST] ranking in management I field: tier II)
(5) P4P design 4: The importance of disease management activities in P4P programs
After 2017, Dr. Chen and his coauthors focused on the disease management activities embedded in the P4P model. They realized that perhaps it was not the excellent incentive design (amount or structure) that could achieve a successful P4P; instead they considered the disease management programs (DMPs) to be the vital key for successful participatory P4P design (see the final paragraph). They first chose two kinds of P4P that have implemented DMPs to different degrees, and checked whether different degrees of DMPs embedded in P4P were associated with better patient outcomes. Finally, they concluded their insights and findings regarding the importance of DMPs based on the chronic care model to write a review.
In 2017, Dr. Chen and his coauthors examined the effect of a P4P program on health outcomes for patients with severe hepatitis B or C. This program did not have more disease management activities involved. They found that P4P has not resulted in reduced negative outcomes or enhanced quality of life (QoL). They suggested the P4P program could strengthen disease management activities/patient-centered care to achieve better patient health outcomes.
Tsung-Tai Chen, Ya-seng (Arthur) Hsueh, Chun-Hsiung Ko, Ling-Na Shih, Sien-Sing Yang*. The effect of a hepatitis pay-for-performance program on outcomes of patients undergoing antiviral therapy. European Journal of Public Health 2017 27(6): 955-960.
(IF=3.367; 2020 SSCI: Public, Environmental & Occupational Health, 44/176 [25%, Q1])
Wei-Chih Su#, Tsung-Tai Chen#, Sien-Sing Yang, Ling-Na Shih, Chih-Kuang Liu, Chia-Chi Wang, Chien-Hsien Wu*. The Effect of a Hepatitis Pay-for-Performance (P4P) Program on Patient Health-Related Quality of Life in Taiwan. (Accepted).
#: equal contributions ([Q2])
In 2019, Dr. Chen and his coauthors examined the effect of another P4P program on health outcomes for patients with schizophrenia. This program included a number of relatively simple disease management activities (e.g. emotional support or reminders) compared to the hepatitis P4P program. They found that although these disease management components/patient-centered care (PCC) features of the P4P program can be beneficial for compulsory admissions and satisfaction, more sophisticated activities, such as health promotion targeting disadvantaged patients, could still need to be implemented to reduce the occurrence of complicated adverse outcomes.
Tsung-Tai Chen, Jing-Jung Yang*, Ya-seng (Arthur) Hsueh, Vinchi Wang. The Effects of a Schizophrenia Pay-For-Performance Program on Patient Outcomes in Taiwan. Health Services Research 2019 54(5):1119-1125.
(IF=3.40; 2020 SSCI: Health Policy & Services, 16/88 [18%, Q1], The Ministry of Science and Technology [MOST] ranking in management I field: tier I)
Tsung-Tai Chen, Ke-Hsin Chueh, Kao-Chen Chen, Chi-Ling Chou, Jing-Jung Yang. The satisfaction of patients with schizophrenia in Taiwan: A cross-sectional survey on patient-centered care domains. Journal of Nursing Research 2022 (Accepted).
(IF=2.517; 2021 SSCI: Nursing, 37/123 [30%, Q2])
In 2021, Dr. Chen and his coauthors published an invited review based on their empirical findings above. They highlighted the importance of disease management activities based on the chronic care model in participatory P4P in Taiwan, which focused on patient engagement and simply rewarded participation in care-improvement activities without necessarily linking bonuses to the attainment of objectives based on specific measures. They discussed the chronic care model (CCM) in relation to the diabetes P4P program in Taiwan since most evidence has shown that the diabetes P4P is beneficial for any patient outcome. They concluded that the successful characteristics of this P4P program in Taiwan include its focus on extrinsic and intrinsic incentives (i.e., shared care network), physician-led P4P and the implementation of activities based on the chronic care model (CCM) components. However, they worried that due to the low rate of P4P program coverage, many patients with diabetes would not be able to enjoy the benefits of CCM-related activities or receive necessary examinations. In addition, the majority of these CCM-related activities are not allotted an adequate amount of incentives; additionally, these activities are mainly implemented in hospitals which, compared to primary care providers, are unable to execute these activities flexibly. All these issues could hinder the advance of diabetes care in Taiwan.
Tsung-Tai Chen*, Brian Oldenburg, Ya-seng (Arthur) Hsueh. Chronic care model in the diabetes pay-for-performance program in Taiwan: Benefits, challenges and future directions. World Journal of Diabetes 2021 May 12(5):578-589 (Invited Review).
(IF=4.56; 2021 SCI: Endocrinology and Metabolism, 62/146 [42%, Q2])
Conclusions and future studies for P4P
Regarding the P4P issues, Dr. Chen and his coauthors have contributed to the effectiveness of embedded disease management programs, incentive design, and unintended consequences. In the future, they will focus more on the different aspects of the P4P-mechanism that affect patient outcomes, especially in regard to the features of patient-centered care (PCC) and disease management programs embedded in P4P.
2 Quality report cards/private performance feedback
Quality report cards represent the public disclosure of hospital performance in terms of process and outcome measures, while private performance feedback represents private disclosure of performance. Dr. Chen and his coauthors focused on the public/private disclosure issue correspondence with measurement development and validity, information design, effectiveness of report cards and risk adjustment design.
(1) Report card design 1: Measurement development
In 2017, Dr. Chen and his coauthors demonstrated how to develop report card measures by using rigorous methods. They employed the modified Delphi method to elicit 7 representative indicators that are suitable for our context and aligned with international standards. The government can utilize the study’s results to develop a pediatric quality report card to improve the quality of pediatric care.
Tsung-Tai Chen*, Kuo-Inn Tsou, Shyh-Dar Shyur, I-Jung Tsai, Wei-Chung Hsu, Kuo-Piao Chung, Li-Ying Huang. The use of modified Delphi method and health insurance database to develop feasible indicators for pediatric quality report card. Taiwan J Public Health 2017 36(6):613-622 (In Chinese, Original Article) (TSSCI).
(2) Report card design 2: Validity of measurement and effectiveness of report cards
In 2019, Dr. Chen and his coauthors started to test the validity of measures in current quality report cards in Taiwan, and took acute myocardial infarction (AMI) process measures as examples. They suggested that the process measures currently used on the AMI report card in Taiwan are valid based on their associations with negative outcomes. In other words, a hospital that achieves high scores on process measures probably also achieves better outcome quality.
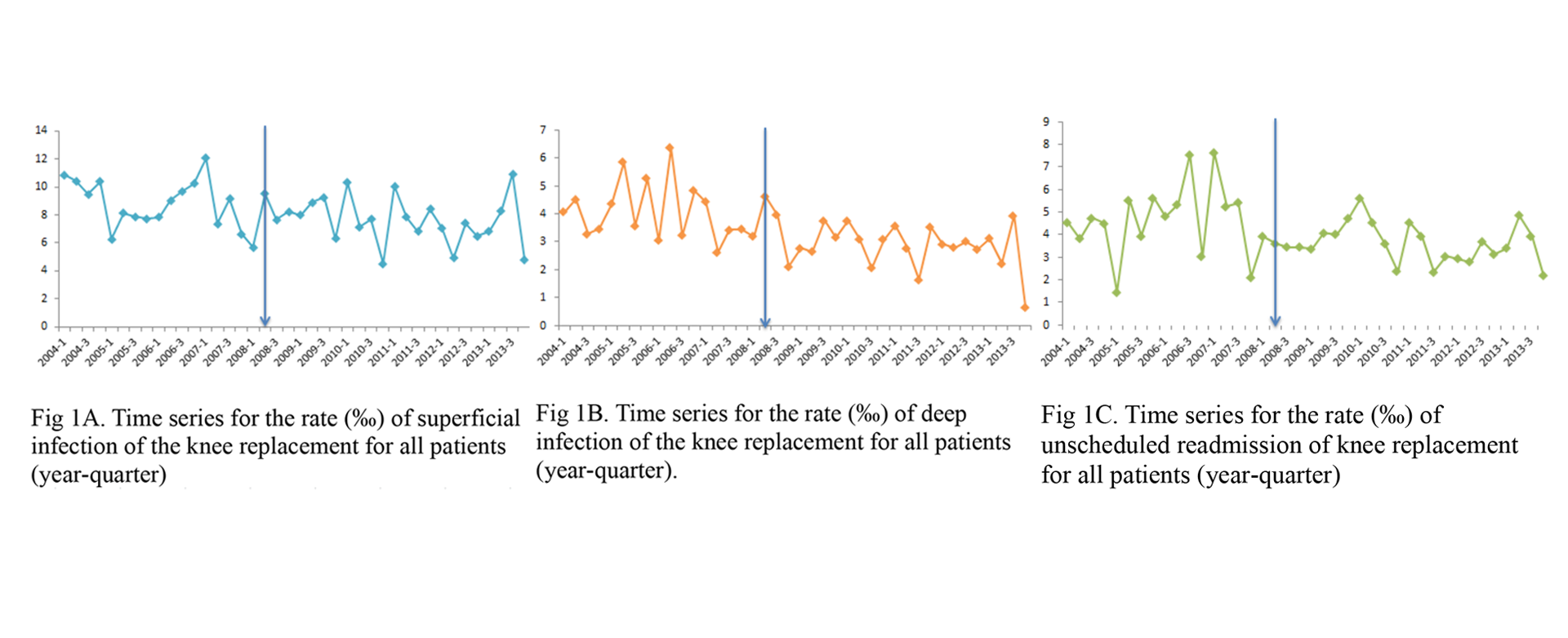
Since the validity of measures in report cards is possibly solid (see the AMI report card above), in 2019, Dr. Chen and his coauthors aimed to find out whether the report card can enhance the quality (effectiveness) if the report card measures are possibly valid. They took a total knee replacement report card (TKR) as an example, and found that the TKR public report card initiative did not improve the rate of infection and unscheduled readmission for surgical site infection. The design of this report card in Taiwan should involve physicians’ participation and should be tailored to be suitable for patients to read in order to further increase the odds of improvement in these negative outcomes.
Tsung-Tai Chen*, Ya-seng (Arthur) Hsueh, Chen-Kun Liaw, Ling-Na Shih, Li-Ying Huang. Does public report card matter? A ten-year interrupted time series analysis on total knee replacement. European Journal of Public Health. 2020, 30(1):4-9.
(IF=3.367; 2020 SSCI: Public, Environmental & Occupational Health, 44/176 [25%, Q1])
Tsung-Tai Chen, Ya-seng (Arthur) Hsueh, Yun-Hua Chen, Hui-Chu Lang, Chieh-Min Fan, Chung-Jen Wei, Tzong-Luen Wang*. Validity of acute myocardial infarction inpatient process measures on the report card in Taiwan: do they vary by outcomes? Taiwan J Public Health 2019 238(3):289-300 (In Chinese, Original Article) (TSSCI).
(3) Report card design 3: Information design
In addition to measure report card design, in 2018, Dr. Chen and his coauthors also focused on information design. They proposed the framework of successful design and then in greater detail described the importance of tailoring patients’ required information along with various considerations for eliciting the information from the patients.
Tsung-Tai Chen*, Kai-Ren Chen, Ming-Hsin, Phoebe Chiu. New generation of quality report card design considerations–patient view of the tailored need for information. Taiwan J Public Health 2018 37(4):366-374 (In Chinese, Reviews) (TSSCI).
(4) Report card design 4: Risk adjustment design
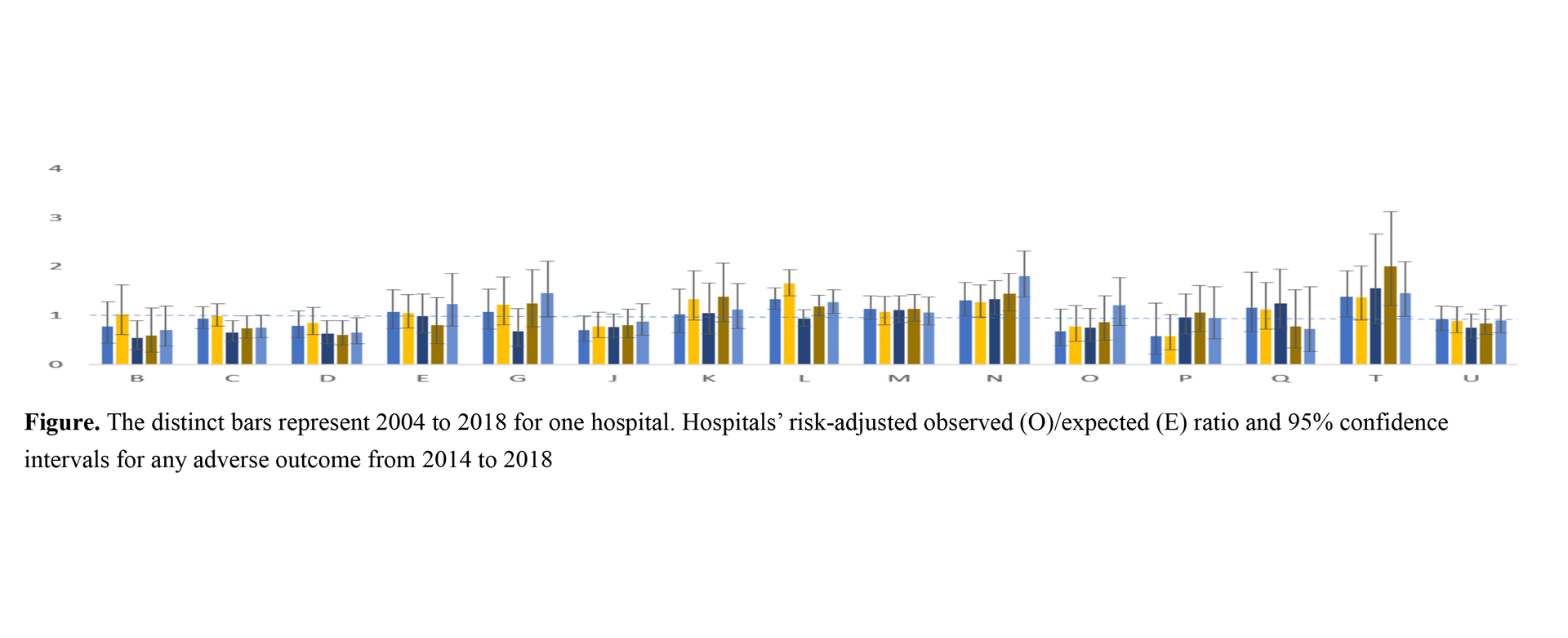
In 2021, Dr. Chen and Prof. Tsou demonstrated how to design risk adjustment in a report card. As a matter of fact, they have assisted the Premature Baby Foundation in Taiwan for several years to help produce profiling reports (private performance feedback) for hospitals participating in the Taiwan Premature Infant Follow-up Network (TPFN), most notably in terms of risk adjustment, which for example considers that hospitals treat more disadvantaged patients, and make adjustments based on the observed performance to make hospital comparison fairer. They concluded that risk adjustment is important, especially for mortality, since the ranks for mortality have the lowest concordance. In addition, they also stated that they cannot come to a definite conclusion regarding whether a hospital is high in quality in preterm care if only 1 or 2 adverse outcomes are taken as profiling measures.
Tsung-Tai Chen, Kuo-Inn Tsou*, Waitim Jime, Chi-Nien Chen. Risk-adjusted rates between hospitals for adverse outcomes of very-low-birth-weight infants. Journal of the Formosan Medical Association 2021 May (21):00138-8.
(IF=3.28; 2020 SCI: Medicine, General & Internal, 53/169[31%, Q2])
Conclusions and future studies for public disclosure
It is true that report card measures can be produced by the Delphi method assisted with administrative claim data. Additionally, according to our research related to the AMI report card, at hospital level, the measures have certain level validity, and hence citizens and physicians could have more evidences in using report cards. However, our research found a lack of effectiveness of report cards on quality improvement, and lower use rates of public report cards (around less than 3% of overall population).* In the future, finding ways to make a report card with tailored information for different kinds of patients is a big challenge. The development of physician rating websites (PRWs) can improve some disadvantages of public report cards, for example, replacement of the complicated clinical measures with patient review; however, the PRWs should integrate these clinical measures from traditional report cards to make a comprehensive and reliable profiling design.
*The unpublished manuscript (submitted)
314 views